M.C. Barrett, Ph.D. • January 12, 2026
Trauma can take many forms. Therapy can help.

Have you survived a life-threatening event and now feel changed as a person? Maybe you’re feeling disconnected from others, disinterested in or angry with the world, or unable to relax. Perhaps it feels like your mind won’t let go of terrible, upsetting memories. These symptoms are common after a traumatic event, and they can also be very disruptive to our everyday life. If any of this sounds familiar to you, know that you are not alone and that psychologists at Aviva Psychology Services are trained to help.
This post will help you evaluate whether a trauma-focused therapy for PTSD may be a good fit for your unique needs and symptoms so you can make an informed decision about your care.
You will learn about the clinical definitions of trauma, common impacts of trauma, disorders like PTSD and CPTSD. You will also learn about the available evidence-based treatments for treating trauma, PTSD, and CPTSD.
First, it can be helpful to know that trauma impacts most adults at some point in their lives, and we are biologically hardwired to have a strong emotional and physical reaction to traumatic experiences. After all, a threat to our well-being is a big deal! A big response makes sense, too, and it can help us survive dangerous situations.
However, even a biologically and psychologically normal reaction can be uncomfortable, can be challenging to manage, and can be difficult to recognize as a trauma response. Our reactions to trauma are as unique as each person who survives trauma and as unique as each experience of trauma. Survivors of trauma often feel disconnected from others, even close loved ones, and often worry that they are doomed to experience their symptoms forever. When experiencing symptoms like these, it can be difficult to connect with others, to complete our usual activities, or even to feel like you’re the same person you were before the trauma occurred.
However, there is good news: many people recover naturally from trauma after a few weeks, and for those that experience persistent symptoms, there are safe, effective treatments that can be completed in just a few months of weekly therapy. Whether your symptoms resolve quickly or more slowly, recovery is possible, and you don’t have to accomplish it alone.
What Exactly Is Trauma?
In everyday life, people use the word “trauma” to describe many different types of experiences. For example, they may refer to going through a divorce, experiencing a life-threatening illness, working in a toxic job environment, and being involved in a car accident as traumatic experiences.
However, in the field of trauma psychology, a traumatic experience has a very specific definition: an experience of actual or threatened death, serious injury, or sexual violence. Sometimes we experience trauma directly, such as surviving a house fire or being assaulted. Other times, however, we experience trauma indirectly. For example, we may learn about a loved one being seriously harmed or killed. Some people also experience trauma indirectly as a recurrent part of their job, such as what is experienced by firefighters, military members, or emergency room workers.
Although we may prefer to believe that traumatic experiences are rare, psychological research tells us that most people—about 70% of adults worldwide—will experience trauma at least once in their lifetime, and many people will experience trauma multiple times throughout their life. This is because trauma can take many forms.
Despite what television and movies may lead us to believe, trauma is not limited to extreme settings and specialized careers, such as war experienced by military personnel. Instead, it often takes the form of everyday life events such as car accidents, occupational hazards, natural disasters like fires or hurricanes, violent crime, and abuse within our relationships. Sometimes people experience trauma as a singular event, but trauma often involves recurrent experiences or occurs over prolonged periods of time. Some examples of prolonged trauma experiences are childhood sexual abuse and intimate partner violence.
It is important to note that as a result of societal biases and structures, not everyone is at equal risk of trauma. Trauma is experienced with greater frequency by individuals who have identities that are marginalized by society. For example, women experience higher rates of trauma than men, LGBTQ people experience higher rates of trauma than heterosexual people, and BIPOC people experience higher rates of trauma than white people. Those with multiple marginalized identities are at the highest risk of experiencing trauma and the highest risk of developing trauma-related mental health conditions.
It is also important to acknowledge that difficult life events that do not meet the definition of “trauma” used by clinical science still have real, profound impacts on us. Trauma is a very specific type of experience, and trauma psychology defines it narrowly to help ensure that trauma-focused therapies are only offered to those who will benefit from them, as PTSD therapies can be harmful to those who do not have the specific histories and symptoms they are designed to treat. However, the specific events that meet the clinical definition of "trauma" are not the only type of experience that matters, that can result in a mental health diagnosis, and that may warrant therapy.
For example, a difficult breakup or divorce or unexpected loss of a job could result in depression. The stress associated with chronic illness or a toxic work environment can result in experiences of anxiety and burnout. Dysfunctional, hurtful, or abusive relationships can change how we connect with ourselves or others and warrant therapy related to relationships. Aviva Psychology Services offers treatment for these experiences and more.
How Does Trauma Affect Us?
Experiences of trauma frequently lead to short-term symptoms while our minds and bodies process the experience. For example, a person who survives a car accident may have nightmares about the incident or feel anxious when in a car for a few weeks. This is natural, but when symptoms persist for longer than a month, it may be time to consider a trauma-focused therapy to help resolve symptoms. These symptoms can take many different forms, often depending on the nature of the traumatic experience itself and the survivor’s unique history.
It’s important to recognize that while PTSD is the disorder most people associate with trauma, psychological research tells us that reactions to trauma may take many different forms and can result in many different diagnoses. Moreover, after a traumatic experience, a person may have relatively mild PTSD symptoms but much more severe symptoms of a different disorder.
For example, following a traumatic loss,grief may persist and require therapy, and grief can eventually develop into
depression that needs treatment, too. Sometimes survivors of sexual assault develop Obsessive Compulsive Disorder, often involving themes related to contamination and safety. Transportation accidents can result in intense, persistent experiences of fear that take the form of
anxiety disorders like phobias. For some people, trauma results in persistent sleep-related symptoms, resulting in a diagnosis of Insomnia. You can
schedule an appointment for evaluation and trauma-informed treatment of each of these conditions as Aviva Psychology services.
People who have experienced trauma may experience the aforementioned conditions instead of PTSD or they may have diagnoses in addition to a condition like PTSD. Because trauma can result in so many different symptoms and diagnoses, meeting with a psychologist who is trained in psychological assessment and differential diagnosis is an important first step in recovery, as determining the correct diagnoses will guide you to the most effective treatments.
What is PTSD?
PTSD is diagnosed when a person experiences a specific combination of trauma-related symptoms that begin after a specific kind of traumatic experience.
The specific kind of traumatic experience that can result in a PTSD diagnosis is an event in which a person experienced actual or threatened death, serious injury, or sexual violence. The person may have experienced the trauma personally, been exposed to the trauma of others repeatedly via their job, or may have learned of a close loved one experiencing violence or accidental death. A person may be diagnosed with PTSD following a single experience of trauma, recurrent trauma, or after experiencing multiple, separate types of trauma.
The symptoms of PTSD fall into four categories. PTSD involves intrusive symptoms (like nightmares and strong emotional responses to trauma reminders), avoidance symptoms (like avoiding thinking about the trauma or avoiding situations that are trauma reminders), changes in our thoughts and mood (like strong feelings of guilt or shame or difficulties with trust), and nervous system hyperarousal (like irritability, difficulty concentrating, or being easily startled).
PTSD is only diagnosed if symptoms have persisted for at least a month following the trauma and if the symptoms are causing problems in multiple areas of life, such as at work, in relationships, or at school. How PTSD interferes with daily life looks different for each person, as every survivor of trauma and every traumatic experience is unique. However, some common examples of PTSD-related disruptions are problems with sexual intimacy, isolating and avoiding to the point that our relationships and responsibilities suffer, recurrent conflict with supervisors at work, and trouble tolerating the uncertainty of daily life events.
What is complex PTSD?
If you’ve spent much time reading about mental health online, you’ve probably heard the term “complex PTSD,” which is sometimes abbreviated as CPTSD. This is a clinical term with a very specific definition. Unfortunately, it is frequently misunderstood by the public and even by healthcare providers who do not have advanced training in trauma and advanced understanding of trauma-related research. There are three especially common myths related to “complex PTSD.”
One common myth is that CPTSD means you have an “especially severe or complicated” presentation of PTSD. In reality, both PTSD and CPTSD exist on a spectrum of severity, trauma-related disorders are not necessarily more severe than other disorders, and trauma-related disorders are not necessarily the most severe outcome after a traumatic experience. For example, after trauma, a person could have minimal PTSD symptoms and severe depression.
A second myth is that CPTSD refers to PTSD from repeated or prolonged trauma. In reality, both both PTSD and CPTSD can be related to single-event trauma or from prolonged or multiple traumatic experiences.
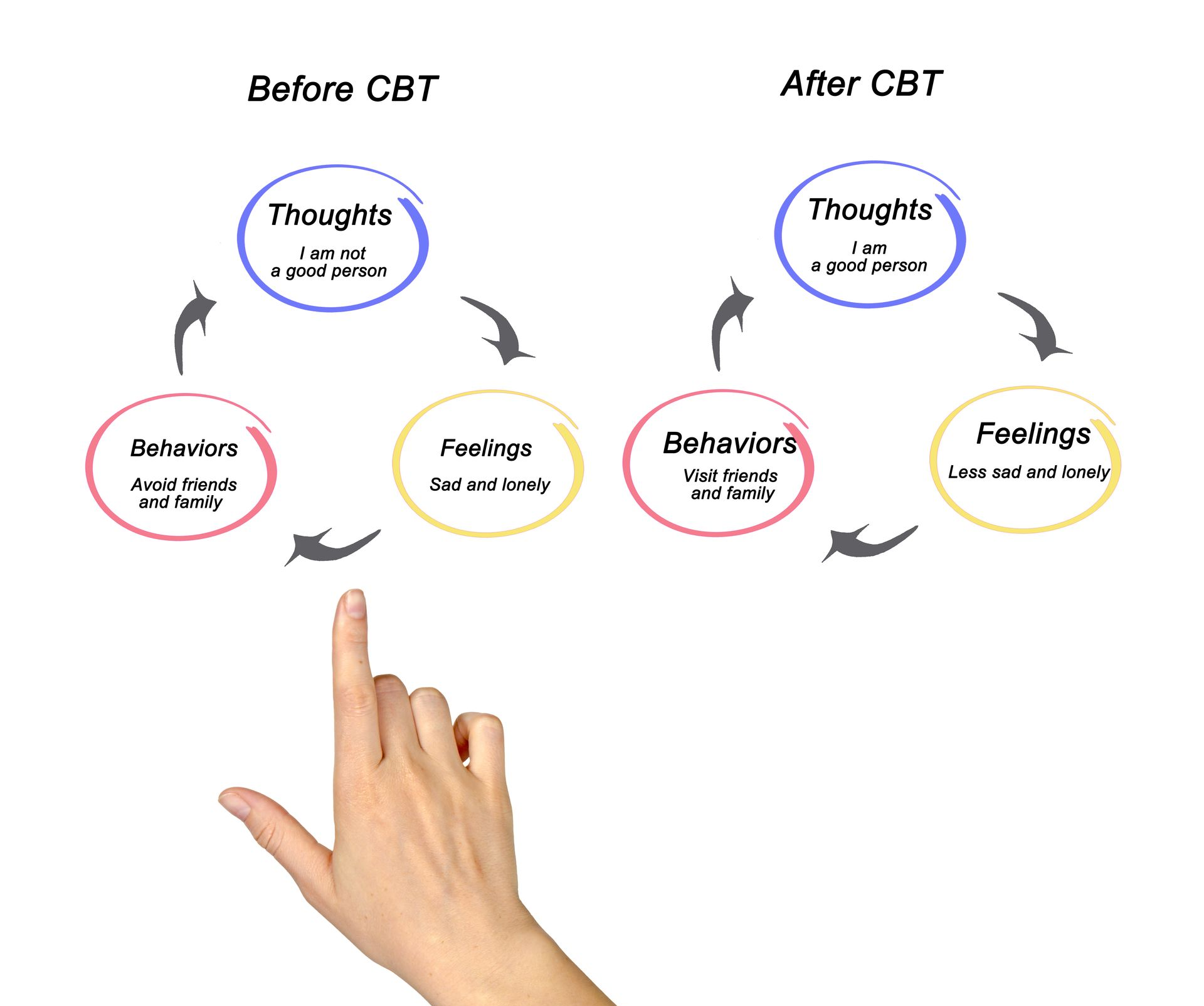
A third myth is that CPTSD should not be treated via standard PTSD therapies. In reality, decades of clinical research have clearly indicated that PTSD and CPTSD are most effectively treated with the same forms of psychotherapy. Specifically, both are most effectively treated via specific types of PTSD-focused Cognitive Behavioral Therapy, with the strongest evidence to support Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE).
To accurately understand PTSD and complex PTSD, it is helpful to first know that there are two main systems for diagnosing mental health conditions. One system is called the Diagnostic and Statistical Manual (or DSM) and is used in the United States. The other is called the International Disease Classification (or ICD) and is used by the rest of the world. Both systems are regularly revised and updated to reflect psychological research findings, but the two systems are not always updated at the same time or in the same way.
The term “complex PTSD” was initially proposed by researchers in 1980 to account for trauma-related symptoms that were not included in the narrow definition of PTSD that was in use by both the DSM or ICD systems at that time. The proposed complex PTSD symptoms included experiences like persistent negative emotions, impulsive behaviors, and multiple forms of difficulty in relationships.
The DSM has had multiple revisions since 1980, and it now defines PTSD more broadly, in a manner that includes many of the symptoms originally proposed as “complex PTSD.” The DSM chose to include the proposed CPTSD symptoms in the standard PTSD definition because research indicated the two have significant overlap and respond best to the same treatments. Therefore, the DSM took an inclusive approach that integrates the two diagnoses and includes the proposed "complex PTSD" symptoms within the definition of PTSD.
The ICD has also been updated multiple times since 1980. However, it has not used the same inclusive approach to defining PTSD. The ICD uses a narrow definition of PTSD and lists a separate diagnosis of CPTSD. The separate CPTSD diagnosis requires an individual to meet all the criteria of PTSD and to additionally meet criteria for separate “complex PTSD” symptoms. This approach is more specific and more exclusionary. As a result, some people with significant trauma histories and symptoms fall “between” the ICD’s narrow definitions of PTSD and CPTSD, resulting in neither diagnosis being given. This is especially problematic for healthcare access in the United States, where insurance companies require diagnoses before paying for treatment like therapy.
What treatments are effective for PTSD?
PTSD and CPTSD have been highly researched for decades. As a result, expert psychologists at the American Psychological Association and at the National Center for PTSD have been able to identify which treatments have the most scientific evidence to indicate that they are safe, effective forms of treatment for PTSD and CPTSD.
There are four evidence-based therapies for PTSD available at Aviva Psychology Services: Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE), which are considered frontline, gold standard treatments for PTSD, as well as Written Exposure Therapy (WET) and Skills Training in Affective and Interpersonal Regulation (STAIR), which are also considered evidence-based for PTSD.
How Much Does Treatment Help?
Many survivors of trauma are skeptical that psychotherapy can help them. PTSD symptoms are intense, overwhelming, and can feel impossible to change.
However, there is strong scientific evidence that PTSD is highly treatable and that the gold-standard, frontline treatments of Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) are highly effective. In fact, psychological research has demonstrated that they are effective for people of all backgrounds, with all different types of trauma, and regardless of how long ago the trauma occurred or whether the trauma involved a one-time event or a long period of exposure to trauma. Research indicates that most people who complete PE or CPT recover so dramatically that they can no longer be diagnosed with PTSD at the end of treatment. Those who still have the diagnosis often still experience very significant improvements in their daily life.
Yet these research findings do not guarantee dramatic improvement for every individual who completes PTSD treatment. This is because there are important individual factors that influence treatment outcomes. One especially important individual factor is treatment engagement: people who attend therapy sessions consistently and complete therapy homework on a daily basis achieve greater improvement in therapy than those who miss sessions or miss homework assignments. Much like physical exercise, one hour a week is likely to only result in minor changes, but daily work can transform a person’s life entirely. Trauma psychologists at Aviva Psychology Services are trained to help clients engage fully and effectively so that they can get the best possible results in treatment.
Another important factor is individual readiness to commit to the full course of trauma therapy, which is safe and effective but an emotionally intense and time-consuming process. Some clients prefer to start with a trauma-informed treatment like STAIR, which is available at Aviva Psychology Services and designed for those with a traditional CPTSD presentation, to boost coping skills prior to doing a more intensive, trauma-focused therapy like CPT or PE. Other clients may have other conditions, such as
anxiety or
depression, that they wish to address prior to trauma-focused therapy, so that they have more capacity for the emotionally challenging work of trauma treatment.
Aviva Psychology Services offers an individualized, flexible approach to treatment and a wide range of treatment options and styles to ensure that your readiness is considered thoughtfully and your therapy experience is as helpful as possible.
How Do I Get Started with Trauma Therapy?
If you think you may benefit from trauma-focused therapy, the first step is getting connected to a provider who has training to assess your symptoms, determine the most accurate mental health diagnoses, and help you build an individualized treatment plan. You can get connected with a psychologist with expertise in trauma by filling out the
Request an Appointment form.
Selected References and Additional Reading:
- American Psychological Association. (2021). Post-traumatic Stress Disorder.
https://www.apa.org/topics/ptsd
- American Psychological Association. (2025). Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults.
https://www.apa.org/ptsd-guideline
- National Center for PTSD, Dept of Veteran Affairs. (2022)
https://www.ptsd.va.gov/understand/what/complex_ptsd.asp
- National Center for PTSD, Dept of Veteran Affairs. (2020).
https://www.ptsd.va.gov/professional/treat/txessentials/complex_ptsd_assessment.asp
- Norman, S., Hamblen, J., & Schnurr, P. (2023). Overview of Psychotherapy for PTSD. National Center for PTSD.
https://www.ptsd.va.gov/professional/treat/txessentials/overview_therapy.asp
- Wall, D. (2021, March 10). Post Traumatic Stress Disorder (PTSD) | Fact Sheet - ABCT - Association for Behavioral and Cognitive Therapies. ABCT - Association for Behavioral and Cognitive Therapies. https://www.abct.org/fact-sheets/post-traumatic-stress-disorder/
SHARE THIS POST:
Our Recent Posts: