M.C. Barrett, PhD • December 29, 2025
Insomnia impacts your whole life. CBT-I therapy can help.

A bad night of sleep can make the next day challenging. When poor sleep quality becomes a persistent problem, the effects on our lives aren’t just inconvenient—they’re harmful. In fact, sleep problems are so disruptive to our daily life that one of the top internet searches about insomnia is, “Can insomnia kill you?”
While insomnia is not a direct cause of death, it is associated with increased risk of other life-threatening conditions, such as heart disease, and insomnia can impair our thinking and behavior, increasing risk of dangerous events like car accidents. Fortunately, there is good news: therapy like Cognitive Behavioral Therapy for Insomnia (CBT-I) has strong research support that tells us it is safe and effective, and psychologists at Aviva Psychology Services are trained to provide it. Best of all, CBT-I can help you make big changes quickly—it usually requires only six to eight weeks of therapy!
Why Is Sleep Important?
Sleep is important not only for feeling energized the next day but for our overall physical and mental health. During sleep, our bodies and brains rest and repair themselves, and when this is interrupted, our functioning declines and we can experience profound suffering. After all, there is a reason that prolonged sleep deprivation is considered a form of torture by international law.
Physically, sleep is an important biological process that plays a vital role in our body’s ability to clear toxins, maintain our immune system’s ability to fight disease and develop immunity, and sustain our body’s regulation of temperature and metabolism. Without regular and restful sleep, our body struggles to maintain these vital functions, leaving us more vulnerable to illness and other physical ailments.
Psychologically, sleep is necessary for learning and memory, emotion regulation, concentration, and our ability to tolerate stress. When we are sleep deprived, we are more sensitive to both physical and psychological pain, our reflexes are slowed, and our decision making is impaired. As a result, sleep deprivation makes it difficult for us to complete many daily activities such as work tasks, driving, parenting, self-care tasks like healthy eating and exercise, and navigating complex emotional challenges like conflict with others.
Chronic poor sleep is also associated with a multitude of negative health outcomes, including increased risk of heart disease, Alzheimer’s and other forms of dementia, increased likelihood of developing mental health conditions like depression and anxiety, being at higher risk of suicide, and an overall shorter lifespan.
What is Insomnia?
Insomnia Disorder, colloquially referred to as insomnia, is diagnosed when certain conditions are met. First, a person must have dissatisfaction with their quality of sleep due to difficulty falling asleep, difficulty staying asleep throughout the night, and/or waking too early in the morning and being unable to return to sleep. Second, sleep problems must be disruptive to other aspects of life, such as functioning at work, in school, or in relationships. If symptoms occur at least three nights per week, have persisted for at least three months, and there are no medical conditions or substance use causing the problem, Insomnia Disorder is likely present. Research tells us that insomnia is quite common and impacts up to 30% of adults.
Sleep difficulties often fall into one of three distinct patterns: short-term, persistent, or recurrent.
For some people, sleep problems are short-term, lasting less than three months. This is a common short-term reaction to stressful life events, such as romantic breakups, experiences of trauma, or grieving the loss of a loved one. This type of sleep problem often resolves naturally, and if people with these experiences seek therapy, typically therapy that focuses on stress, depression, grief, or trauma is the best fit, rather than therapy for the sleep problem itself.
For others, however, insomnia is persistent and may require treatment that directly addresses sleep. Chronic insomnia can last for many months or even years without remission, resulting in chronic fatigue and difficulties and radically altered lifestyles. Insomnia can also “come and go” as recurrent episodes of three months with periods of remission between episodes.
What Causes Insomnia?
Insomnia is sometimes categorized as either primary insomnia or secondary insomnia. Primary insomnia means that the insomnia is not being caused by a medical condition, medication side effect, mental health condition, or life circumstance. Simply put, primary insomnia means the problem is only sleeplessness.
However, most people with insomnia experience secondary insomnia. This means that for most people, insomnia is caused by or is occurring at the same time as another condition. For example, secondary insomnia can be related to medical conditions like Long COVID, sleep apnea, asthma, Alzheimer’s disease, or chronic pain. Mental health conditions like depression, anxiety, and PTSD are also associated with insomnia. Hormonal concerns, such as thyroid conditions and menopause, also commonly impair sleep. Many substances can cause sleep problems as a side effect, including prescription medications, recreational drugs, and alcohol.
Insomnia can also be a result of life circumstances. For example, having a new baby results in nighttime parenting duties that make getting a good night of sleep challenging. Another factor can be not having a comfortable place to sleep, such as lacking air conditioning during hot weather or having a bed partner who has their own sleep problems like snoring or restlessness. Stressful life experiences, such as divorce, job loss, trauma, or grief also impact our ability to sleep regularly and restfully.
While anyone can develop insomnia, research tells us that there are certain risk factors. Women are more commonly affected by insomnia than men, with research indicating more than one in four women in the United States have insomnia. The risk of insomnia is also higher for older women than younger women. At this time, researchers aren’t sure why women are at higher risk of insomnia than men, but current theories include hormonal fluctuations associated with menstruation and menopause.
Other risk factors for insomnia include high levels of stress, having a mental health condition like depression, anxiety, or PTSD, and living with chronic illnesses such as sleep apnea, long COVID, chronic pain, or asthma.
What Treatments for Insomnia Are Available?
Broadly speaking, sleep difficulties like insomnia can be treated in two ways: with medication and with therapy. Medications are often highly appealing as a potential quick, easy solution. Unfortunately, research indicates that medications are not ideal for treating insomnia.
This is especially true for over-the-counter medications like antihistamines, some of which can cause significant medical problems such as increased risk of dementia when misused for their sedative effects. Medications commonly prescribed by physicians to help with sleep, such as melatonin, trazodone, and benzodiazepines like xanax or klonopin, have also been found to have limited research support. In fact, they are considered to have “weak evidence against” their use for insomnia, per the 2025 Clinical Practice Guidelines for Insomnia published by the US government. These guidelines are issued routinely, based on large-scale research conducted by national experts, and are considered a leading source of treatment guidance for healthcare providers.
However, the 2025 Clinical Practice Guidelines indicate “strong evidence for” Cognitive Behavioral Therapy for Insomnia (CBT-I). CBT-I is considered an evidence-based therapy, which means there is robust research to support that it is a safe and effective treatment. In fact, it is considered the first-line treatment for both short-term insomnia and chronic insomnia. Most individuals who complete a full course of CBT-I see significant improvement in their quality of sleep.
What Does CBT for Insomnia Involve?
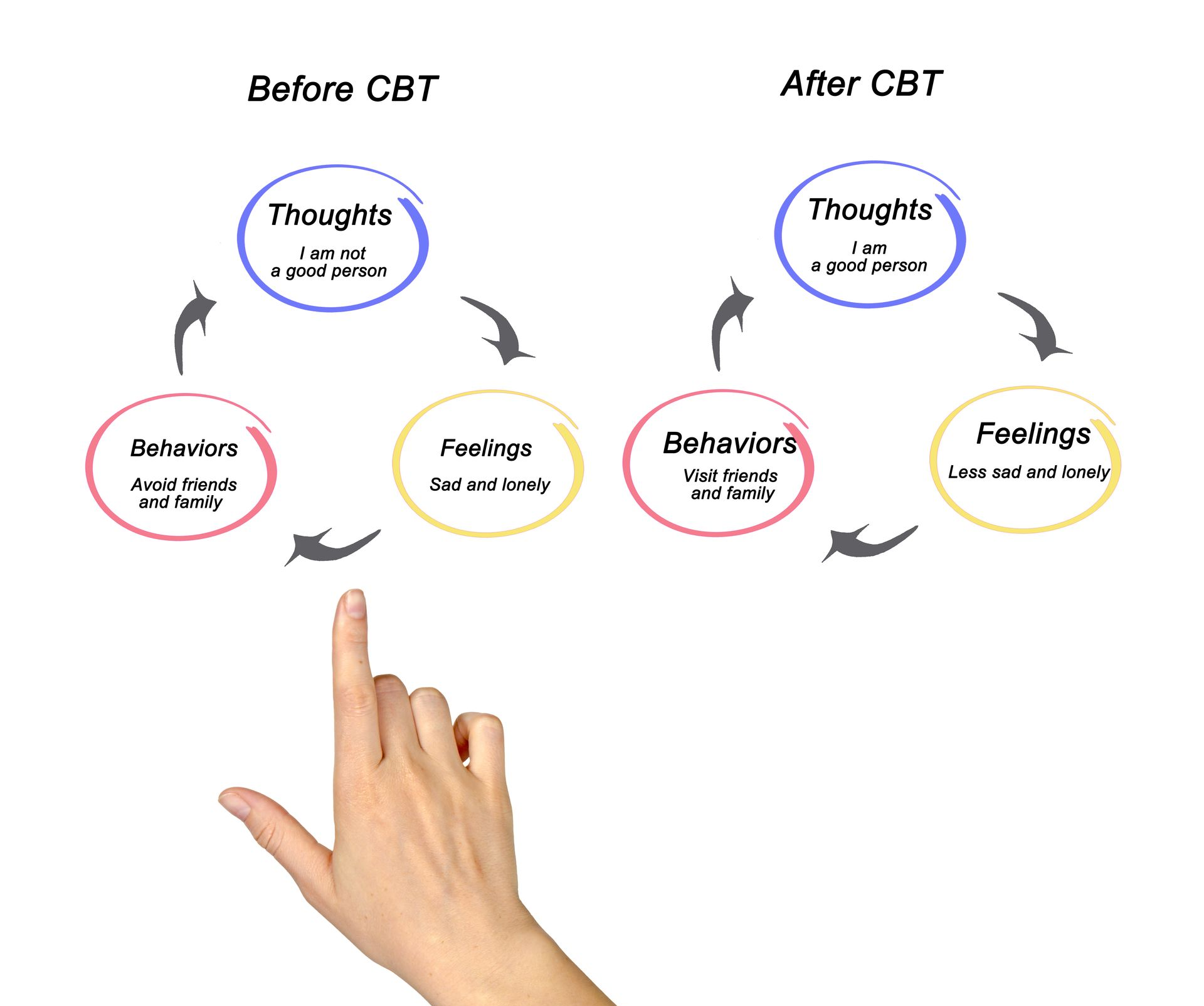
CBT-I is a highly structured approach to therapy that involves completing a specific therapeutic program to improve sleep knowledge, sleep habits, and coping strategies for managing sleep. It is a short-term therapy, often completed in only six to eight weekly sessions. As a form of cognitive behavioral therapy, it focuses on understanding and changing thoughts and behaviors.
In CBT-I, patients are taught about the science of sleep so that they can learn to become their own sleep manager after the therapy concludes. The treatment emphasizes developing healthy sleep habits, such as maintaining a regular sleep and wake time and not spending too much time awake in bed. CBT-I also utilizes relaxation techniques, such as breathing exercises and progressive muscle relaxation, to help patients increase the odds that they will experience efficient sleep. Lastly, CBT-I involves using techniques of sleep restriction and/or sleep compression. These strategies help patients first consolidate their sleep into continuous hours of higher-quality rest, then gradually prolong their duration of sleep.
Completing CBT-I can be challenging, as changing habits and restricting our sleep to “reset” our sleep schedule is an uncomfortable process. However, research tells us that while there is discomfort in this process, the discomfort does not last long and the process is not dangerous. In fact, CBT-I is considered the front-line treatment for insomnia, meaning it’s the best treatment science has developed so far!
How Do I Begin Therapy for Insomnia?
If you are dealing with the disruptive effects of insomnia, rest assured that CBT-I can help you get better rest. CBT-I is a safe, effective treatment that can help you make significant changes in your sleep quality quickly, and psychologists at Aviva Psychology Services are trained to help. You can get connected with a psychologist who has expertise in sleep and insomnia by filling out the Request an Appointment form.
Selected References and Additional Reading:
- K.C. Simon, L. Nadel, & J.D. Payne, The functions of sleep: A cognitive neuroscience perspective, Proc. Natl. Acad. Sci. U.S.A. 119 (44) e2201795119,
https://doi.org/10.1073/pnas.2201795119
- National Institute of Health: National Heart, Lung, and Blood Institute. (2022). Insomnia - what is insomnia? Www.nhlbi.nih.gov.
https://www.nhlbi.nih.gov/health/insomnia
- Newsom, R. (2024). Cognitive behavioral therapy for insomnia (CBT-I): An Overview. Sleep Foundation.
https://www.sleepfoundation.org/insomnia/treatment/cognitive-behavioral-therapy-insomnia
- U.S. Dept of Health and Human Services, Office on Women’s Health. (2017). A-Z Health Topics: Insomnia. Retrieved from:
https://womenshealth.gov/a-z-topics/insomnia
- VA/DOD Clinical Practice Guideline. (2024). Management of Chronic Insomnia Disorder and Obstructive Sleep Apnea Work Group Washington, DC: U.S. Government Printing Office. Retrieved from:
https://www.healthquality.va.gov/guidelines/CD/insomnia/index.asp
- Vgontzas AN; Liao D; Pejovic S; Calhoun S; Karataraki M; Basta M; Fernández-Mendoza J; Bixler EO. Insomnia with short sleep duration and mortality: the Penn State Cohort. SLEEP 2010;33(9):1159-1164.
- Wall, D. (2021, March 10). Insomnia | Fact Sheet - ABCT - Association for Behavioral and Cognitive Therapies. ABCT - Association for Behavioral and Cognitive Therapies.
https://www.abct.org/fact-sheets/insomnia/
- Winokur, A. (2015). The Relationship Between Sleep Disturbances and Psychiatric Disorders: Introduction and Overview . Psychiatric Clinics of North America; 38(4): 603-614.
- Zhang, B, Wing, Y.K. (2006). Sex differences in insomnia: a meta-analysis. Sleep: 29(1): 85–93.
SHARE THIS POST:
Our Recent Posts: